Ivane Javakhishvili Tbilisi State University
Paata Gugushvili Institute of Economics International Scientific

ARTIFICIAL INTELLIGENCE AND THE CHALLENGES OF GEORGIA’S HEALTHCARE SYSTEM: PROBLEMS AND DEVELOPMENT PERSPECTIVES
Annotation. Healthcare is one of the most important and advanced areas for the economic and social well-being of both the individual and society as a whole. In Georgia, this sector deserves special attention, because billions have been spent in this direction over the years, although the results obtained are often unsatisfactory and cannot ensure the improvement of the health status of the population. The following problems still remain: the existence of a unified medical information base, the quality of services, the qualification of medical personnel, their motivation, productivity, the shortage of nurses and other low-level service personnel, and the lack of infrastructure.
The aim of the paper is to discuss what are the main problems that prevent the desired results from being achieved, what institutional and economic barriers hinder efficiency, and how a number of issues can be solved with the help of artificial intelligence. Modern world experience shows that despite the short period of implementation of artificial intelligence, it has real potential for transforming the healthcare system. This technology has the power to increase the accuracy of diagnostics, reduce financial costs, improve access to services, ensure the development of personalized medicine and, which is one of the biggest problems in this direction, to collect, analyze and make information transparent.
The work also pays close attention to the potential impact of artificial intelligence in healthcare on the labor market. Traditional approaches are changing, standards and skills that are proven today are losing their relevance in the future. For Georgia and similar countries, this process is both painful during the transition period and vital, as the education system and labour market struggle to keep pace with the rapid pace of technological development.
The article reflects both global trends and the specific reality of Georgia and accordingly offers recommendations: timely reform of the education system, strengthening of digital infrastructure, development of legal and ethical framework regulations, development of digital infrastructure necessary partnership between the state and the private sector. The intelligent integration of artificial intelligence can become not only a technological innovation but also a solid foundation for the country's economic and social progress.
Keywords: Artificial intelligence; healthcare; Georgian economy; innovations; digital transformation; labor market; skills shortage; health policy; data analysis; personalized medicine
Introduction
Healthcare is one of the most important social and economic sectors of the state. It is what determines the health of the population, its working capacity, productivity and, ultimately, the quality of life. When we talk about economic development, we often forget that the economy is ultimately built on individuals, their skills and the resources that each person brings to the labor market. It is impossible to achieve sustainable prosperity if we cannot ensure the improvement of the health of the average working person, as this is directly related to the increase in productivity and its share of efficiency in the economy.
According to the OECD (2020) report, more than 9% of GDP is spent on healthcare globally, although the effectiveness of these expenditures varies significantly across countries. The World Health Organization (WHO) 2022 assessment shows that increased investments in healthcare in developed countries are directly related to increased life expectancy and expanded access to services.
In Georgia, despite the fact that budgetary expenditures on healthcare are increasing annually and billions of GEL are spent, the efficiency of the system is still low. The problem here is not only in finances. The main barrier lies in the weak data management system, the mismatch between education and labor markets, and the lack of strategic vision. In this regard, institutional analysis is particularly important: institutions can be inclusive or extractive, which determines the sustainability and development potential of the economic system (Acemoglu & Robinson, 2012; Arnania-Kepuladze, 2014). In the case of Georgia, the signs of extractive institutions are more evident in the healthcare sector: high costs against the background of low efficiency, the lack of a unified database and analytics, which further complicates the management of the system and seeing the real picture.
The research shows that the problems are multifaceted and include:
• Low remuneration of medical staff, which remains one of the main reasons for demotivation;
• Mismatch of skills and education, which prevents new staff from integrating into the labor market;
• Low level of digitalization, which hinders the management of clinics and the development of data-based policies;
• Shortage of nurses, especially in the regions, which reduces the quality of services;
• Lack of a long-term strategy, which leaves the system without a clear path for development.
These findings are fully consistent with international studies: Harris and Nguyen (2019) indicate that low salaries and limited career opportunities significantly reduce the retention of medical staff; Clark and Patel (2018) emphasize that low level of digitalization remains a weakness of the system in developing countries; Lopez and Murray (2021) believe that the lack of strategic vision is one of the most serious threats to the sustainability of healthcare.
Global experience shows that one of the most effective ways to address these challenges is the integration of artificial intelligence (AI). According to the McKinsey Global Institute (2021), AI can save up to 10% of healthcare costs, improve the quality of services, and enhance patient safety. If, at the clinical level, artificial intelligence is already used in radiology, pharmacy, and personalized treatment, its potential at the state policy level is even broader: creating a national database, predicting workforce needs, and improving the quality of services in the regions.
Thus, the main problem of the Georgian healthcare system is not only a lack of financial resources. The main barrier is the lack of a unified database and strategic analytics, which prevents effective management and long-term planning of the system. It is in this context that artificial intelligence acquires special importance, both as a tool for governance and economic and social development.
Main results
The analysis of the Georgian healthcare system identified three main barriers, overcoming which is critically important for increasing the efficiency of the system. These barriers are related to the absence of a unified database, the shortage of workforce planning and skills, and the inequality in the quality of diagnostics and treatment across regions. It is on these problems that the following analysis is built, showing how artificial intelligence can become a turning point in the process of solving them.
Absence of a unified database and the role of artificial intelligence
One of the main problems of the Georgian healthcare system is the absence of a unified, integrated database. Today, medical information is fragmented: various clinics, polyclinics, and state agencies collect data independently. This creates several serious obstacles:
• The complete patient history is not fully available;
• Duplication of examinations and analyzes is frequent, which increases costs and reduces efficiency;
• The state does not have a clear picture of the health status of the population, which is why policy planning is carried out unsystematically.
• Irrational distribution of financial resources and failure to prioritize
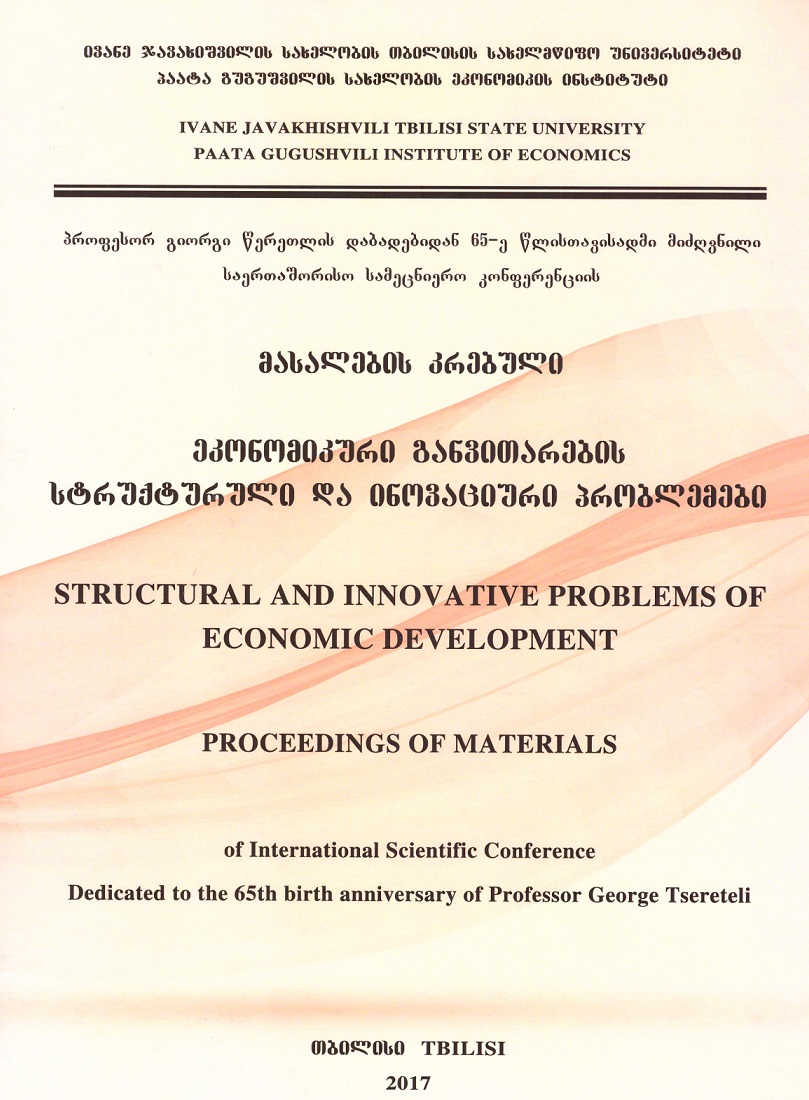
Figure 1: Challenges in the process of hiring new staff
Source: Built by the authors according to the data collected from private survey.
According to the authors’ research, 48% of clinic managers believe that the low level of data management systems creates a serious obstacle to the effective functioning of healthcare, while 23% of representatives of professional associations believe that the introduction of data analytics platforms would significantly improve the quality of services. Similar conclusions were drawn by Clark and Patel (2018), who emphasize that the low level of digitalization in developing countries remains a systemic weakness.
The introduction of a unified electronic health record (EHR) platform would significantly reduce this problem. Such a system would provide:
• Integration of complete patient history, diagnosis, and treatment data into a single database;
• Real-time epidemiological monitoring and optimal service planning;
• Use of predictive analytics to assess disease dynamics and trends;
• Reduction of budget costs by avoiding unnecessary services and targeting resources.
International experience confirms the effectiveness of this approach: in Estonia, where the system is based on data integration, high-quality services have been achieved with relatively small resources. In the US, Medicare uses analytical tools that allow the state to timely assess workloads and plan costs.
Workforce planning and skills balance
The second important problem of the healthcare system is related to the weakness of workforce planning and skills shortages. There is no clear calculation of how many and what profile of doctors, nurses and other specialists will be needed in the next 5–10 years. The education system is unable to synchronize with real demand, which is why both the shortage of personnel and their uneven distribution between regions and cities are growing.
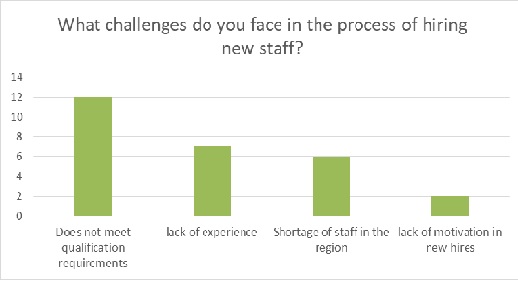
Figure 2: Biggest challenge after employment
Source: Built by the authors according to the data collected from a private survey.
The authors research revealed:
• Low pay: For 72% of newly employed doctors and nurses, the main demotivator was low wages (on average 1,108 GEL for doctors, and in the regions for nurses, less than 500 GEL).
• Mismatch between education and employment: 55% of medical students were only partially informed about the stages of professional development, and 20% were not informed at all. 45% of newly employed people noted that their expectations and reality did not match when they were employed.
• Shortage of nurses: 37.5% of the staff are already over 50 years old, which indicates that the shortage will worsen in the coming years. According to 63% of clinic managers, the lack of nurses directly reduces the quality of service.
This data is consistent with Harris and Nguyen’s (2019) research, which states that low salaries and limited career opportunities significantly reduce the retention of medical personnel. Lopez and Murray (2021) emphasize that the lack of long-term workforce planning leads to a systemic crisis.
By integrating AI, the state will be able to calculate the necessary resources in advance:
• Labor Market Simulation: Based on existing demographic data and morbidity statistics, it can be calculated how many specialists will be needed for different profiles (for example, geriatrics, oncology, mental health).
• Gap Analysis: It will be possible to identify deficient skills, which will allow the education system to adapt to needs in a timely manner.
• Support for education reform: Data-based analytics will help universities and colleges plan the right recruitment and retraining programs.
International experience is also interesting in this regard: the British NHS uses predictive models to determine future needs, and in Japan, where the population is ageing rapidly, analytics are widely used to predict the demand for geriatric medicine personnel.
Quality of diagnostics and treatment in the regions
The third serious challenge is related to the quality and accessibility of services between the capital and the regions. Clinics in Tbilisi enjoy more modern infrastructure and qualified staff, while the population in the regions often does not receive timely and high-quality diagnostics. This leads to late detection of diseases, difficulty in treatment, and additional costs for both families and the state.
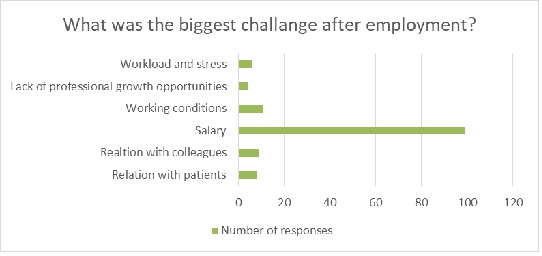
Figure 3: Difficulties in finding specialists in nursing and related fields
Source: Built by the authors according to the data collected from a private survey.
According to the authors’ research, 63% of clinic managers believe that the shortage of nurses in the regions directly reduces the quality of service. Added to this is the infrastructural lag and lack of technological services, which is why patients are forced to travel to the capital for medical care.
Similar trends are described in the WHO (2022) report, which emphasizes that regional inequality is one of the most serious challenges. Lopez and Murray (2021) indicate that the geographical difference in services causes not only social, but also economic losses.
The integration of artificial intelligence into regional healthcare would significantly alleviate this problem:
• Telemedicine platforms: It will be possible to interpret images and laboratory data remotely, which reduces the need for patient movement.
• Decision Support Systems: Doctors will be able to receive accurate and quick recommendations when assessing the patient's condition.
• AI-chatbots and assistants: Primary advice and recommendations will be available to the population, which will prevent delayed diagnosis.
• Predictive Analytics: It will be possible to identify high-risk regions and allocate targeted resources.
From world experience, it is worth noting the e-health platforms of India, which significantly reduce the cost of patient travel to villages; telemedicine systems in the Canadian north, which complement the lack of local clinics; and the unified electronic system of Estonia, which has significantly reduced regional disparities.
The effectiveness of the Georgian healthcare system is most hampered by data fragmentation, insufficient workforce planning, and regional disparities. Proper integration of artificial intelligence in these areas will create a solid foundation for the formation of a unified information system, forecasting personnel demand and supply, and improving the quality of services in the regions. If these three areas are successfully developed, the state will be able not only to allocate the budget more effectively, but also to strengthen the sustainability of the system and public trust.
Conclusions and Recommendations
The study revealed that the main barriers to the Georgian healthcare system are related to the absence of a unified database, a shortage of workforce planning and skills, and disparities in the quality of services across regions. These problems not only reduce the effectiveness of the system, but also significantly increase the disproportionality of budget spending. The current situation shows that increasing financial resources alone is not enough. Structural and technological transformation is necessary, which will enable the healthcare system to become result-oriented and sustainable.
The integration of artificial intelligence can become a turning point in addressing these challenges. AI can provide unification of data systems, predict workforce needs, and reduce regional disparities. International experience (for example, the UK NHS, Estonia’s digital health, telemedicine in the northern regions of Canada, e-health platforms in India) shows that data-driven analytics and the use of innovative technologies significantly increase efficiency and reduce costs.
In this context, it is recommended for Georgia to:
• Create a unified national database that will integrate electronic health records and provide real-time monitoring with AI analytics;
• Forecast workforce needs and synchronize the education system using Labor Market Simulation and Gap Analysis tools;
• Reduce regional disparities using telemedicine platforms and AI diagnostic tools, which will allow the rural population to access services in a timely manner;
• Review the remuneration and motivation policies of medical personnel to ensure sustainable staff retention and development;
• Developing a long-term state strategy that includes technology integration, education reform, and innovation support;
• Strengthening private-public sector partnerships to share international experience and attract investments.
Thus, if artificial intelligence is integrated into the Georgian healthcare system and a strategic vision is developed in parallel, it will be possible to use the budget more effectively, increase the quality of services, and develop the system sustainably.
References
- Arnania-Kepuladze, Tamila. 2018. “Labour Market as a System of Formal and Informal Institutions.” World Science 3 (6): 38–43. https://doi.org/10.31435/rsglobal_ws.
- Clark, Peter, and Ravi Patel. 2018. “Digital Health Challenges in Developing Countries.” International Journal of Medical Informatics 112: 68–75. https://doi.org/10.1016/j.ijmedinf.2017.12.014.
- Harris, John, and Thao Nguyen. 2019. “Healthcare Workforce Retention in Low- and Middle-Income Countries.” Journal of Global Health Studies 5 (2): 77–92. https://doi.org/10.35500/jghs.2019.5.2.77.
- Lopez, Maria, and Samuel Murray. 2021. “Strategic Workforce Planning in Healthcare: Addressing Future Shortages.” Health Policy Review 14 (3): 201–15. https://doi.org/10.1016/j.hpr.2021.03.004.
- McKinsey Global Institute. 2021. Transforming Healthcare with AI: The Future of Data-Driven Medicine. New York: McKinsey & Company.
- OECD. 2020. Health at a Glance 2020: OECD Indicators. Paris: OECD Publishing. https://doi.org/10.1787/4dd50c09-en.
- World Health Organization (WHO). 2022. European Health Report 2022. Copenhagen: WHO Regional Office for Europe. https://apps.who.int/iris/handle/10665/353957.